
Percentage of older adults in the U.S. who felt depressed stressed, or nervous for several days or more within the past two weeks as of January 2021
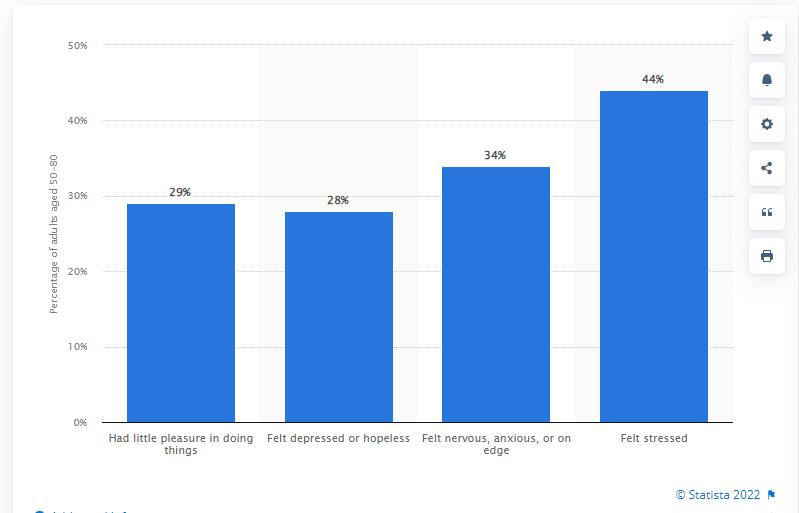
According to Statista, in January 2021, around 28 percent of adults aged 50-80 years felt depressed or hopeless for several days or more within the past two weeks. Moreover, 44 percent reported feeling stressed. This statistic displays the percentage of older adults in the U.S. who felt depressed, stressed, or nervous for several days or more within the past two weeks as of January 2021.
Other poll findings:
- Thirty-seven percent of older adults who say their health is poor reported feeling a lot of stress, compared with just 12% of those who say their health is excellent or very good.
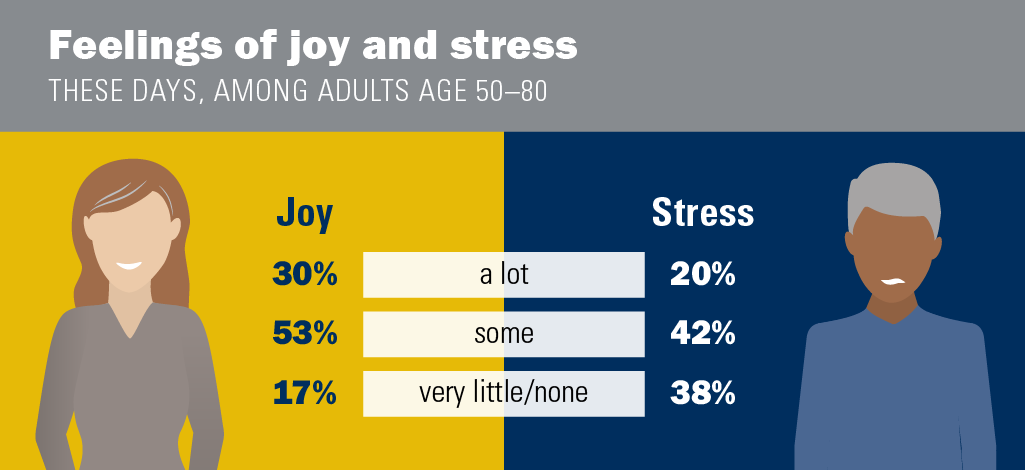
- Twenty percent of older adults say they feel a lot of stress these days, while 38% said they have little to no stress. Those aged 50 to 65 were nearly twice as likely as those aged 65 to 80 to said they experience a lot of stress (25% vs. 13%).
- Seventeen percent of older adults polled said they feel little or no joy these days, but 53% said they feel some joy and 30% say they are feeling a lot of joy.
Current levels of joy and stress
Most adults age 50–80 reported feeling a lot (30%) or some (53%) joy these days, while 17% reported feeling very little or no joy. Meanwhile, 20% of older adults reported feeling a lot of stress these days and 42% felt some stress, whereas 38% felt very little or no stress. Adults age 50–64 were more likely to report feeling a lot of stress compared to those age 65–80 (25% vs 13%), as were women compared to men (24% vs 15%). About half of older adults (47%) said they felt both joy and stress (a lot or some for both).
Older adults in excellent or very good physical health were much more likely to report feeling a lot of joy compared to those in fair or poor physical health (44% vs 16%), and less likely to report feeling a lot of stress (12% vs 37%). Similarly, those with excellent or very good mental health were much more likely to report feeling a lot of joy compared to those in fair or poor mental health (43% vs 4%) and less likely to report feeling a lot of stress (8% vs 62%). Those in the lowest income households (<$30,000) were more likely than those in the highest income households (>$100,000) to have experienced a lot of stress (26% vs 18%) and less likely to report feeling a lot of joy (21% vs 33%).
Paper cited: National Poll on Healthy Aging poll report
