Park et al., (2022)
Park BS, Jin S, Kim WY, Kang DS, Choi YJ, Lee YS. Comparison of the effects of cranial electrotherapy stimulation and midazolam as preoperative treatment in geriatric patients: A CONSORT-compliant randomized controlled trial. Medicine (Baltimore). 2022 Sep 2;101(35).
Funding Source, Location of Study or Author’s Affiliation
This study was conducted at the Department of Anesthesiology and Pain Medicine, Ansan Hospital of Korea University College of Medicine. The protocol was approved by the hospital’s institutional review board (2020AS0142) and registered at the Clinical Research Information Service (KCT0006110). Written informed consent was obtained from all patients participating in this study.
Device
Alpha-Stim 100®
Key Variables
Anxiety
Objective
To observe and compare the clinical effect of cranial electrotherapy stimulation (CES) and midazolam as preoperative treatments in geriatric patients.
Design
Initially, 90 patients were recruited, but 10 patients were withdrawn either spontaneously or in accordance with the exclusion criteria. In this study, 80 patients were included and randomly divided into 2 groups using a computer-generated randomization method: midazolam premedication group (M group, n = 40) and CES pretreatment group (CES group, n = 40). Preoperative anxiety was measured using the 5-point Likert scale, with anxiety levels rated from “Not at all” to “Severe”. The sedation score was assessed using the Ramsay sedation scale, which is a 6-point scale with sedation scores rated from “Anxious and agitated” to “Patients exhibit no response”. Vital signs that were measured include: Systolic and diastolic blood pressure (SBP & DBP), mean arterial pressure (MAP), heart rate (HR), and peripheral capillary oxygen saturation (SpO2). Different investigators performed pre-anesthesia visits, assessment of preoperative anxiety scores and sedation levels, midazolam premedication, CES pretreatment, and anesthesia induction.
Primary Outcome Measure
All measures were assessed three times: (1) on the day before surgery; (2) in the pre-operative holding area on the day of surgery; and (3) after entering the operating room.
- Anxiety was evaluated via 5-point Likert scale:
- 5-point Likert scale (1) indicates “not at all”, (2) “mild”, (3) “intermediate”, (4) “moderate”, and (5) “severe”.
- Sedation score was assessed using the Ramsay sedation scale.
- On a 6-point scale (1) indicates “Anxious and agitated, or restless, or both”, (2) “cooperative, oriented, and tranquil”, (3) “responds to commands only”, (4) “brisk response to light glabellar tap or loud auditory stimulus”, (5) “sluggish response to light glabellar tap or loud auditory stimulus”, and (6) “patients exhibit no response”.
Secondary Outcome Measure
All measures were assessed three times: (1) on the day before surgery; (2) in the pre-operative holding area on the day of surgery; and (3) after entering the operating room.
- Vital signs were measured:
- Systolic and diastolic blood pressure (SBP & DBP), mean arterial pressure (MAP), heart rate (HR), and peripheral capillary oxygen saturation (SpO2).
Key Inclusion Criteria
Eligible patients were
- Aged 65 to 79 years old
- American Society of Anesthesiologists Physical Status Classification II or III
- Scheduled for elective surgery under general anesthesia.
Key Exclusion Criteria
The exclusion criteria included
- Psychiatric medications,
- Obesity (body mass index >30 kg/m2)
- Chronic alcoholism, liver cirrhosis
- Serious renal disease
- Endocrine or neuromuscular disease
- Arrhythmia
- Pacemaker or pulmonary disease.
Protocol Summary
In this study, 80 patients were included and randomly divided into 2 groups using a computer-generated randomization method: midazolam premedication group (M group, n = 40) and CES pretreatment group (CES group, n = 40). Pre-anesthesia visits, assessment of preoperative anxiety scores and sedation levels, midazolam premedication, CES pretreatment, and anesthesia induction were performed by different investigators.
The anxiety score, sedation score, and vital signs (systolic and diastolic blood pressure, mean blood pressure, HR, and oxygen saturation) were assessed three times: on the night before (baseline) and on the day of the surgery in the preoperative holding area (PHA) and in the operating room (OR) before anesthesia induction.
The patients in the M group were intramuscularly injected with midazolam (0.07 mg/kg) 30 minutes before receiving general anesthesia, whereas the patients in the CES group received 20 minutes of CES pretreatment on the day before and on the morning of the surgery. A microcurrent stimulator (Alpha-Stim 100®; Electromedical Products International, Inc., Mineral Wells, TX) was used.
Anesthesia was induced with intravenous injection of propofol (2.0mg/kg) and rocuronium (0.9mg/kg). Three minutes of mask ventilation with sevoflurane administration (3 vol%) at an oxygenated air flow of 8 L/min and a fraction of inspired oxygen of 1.0 was performed before intubation.
Device Application Protocol
The electrode clips of the microcurrent stimulator were attached to the patient’s earlobe, and the microcurrent was adjusted to the power of which the patient experienced light dizziness and a tingling sensation. The power of the microcurrent was limited between 200 μA and 0.5 Hz. All patients were premedicated via intramuscular injection of glycopyrrolate (0.005 mg/kg) 30 minutes before receiving general anesthesia.
Statistical Analysis Plan
The SPSS software version 25.0 for Windows (SPSS Inc., Chicago, IL) was used for statistical analysis. All data except sex were presented as the mean ± standard deviation. Demographic data were analyzed using either the Mann–Whitney U test, the independent t test, or the chi-square test. A p-value of <.01 was considered statistically significant after Bonferroni correction. The preoperative anxiety score and sedation score were analyzed via the chi-square test. A p-value of <.05 was considered statistically significant. Vital signs of each group on the night before surgery, on the day of the surgery in the PHA, and in the OR before anesthesia induction were analyzed via the Mann–Whitney U test or the independent t test. A p-value of <.0033 was considered statistically significant after Bonferroni correction.
The preoperative anxiety score and sedation score were analyzed via the chi-square test. A p-value <.05 was considered statistically significant.
Results
Subjects
A total of 80 patients, with 40 in the CES group, including 21 males and 19 females with a mean age of 69.3± 3.6 years. The M group included 40 subjects, including 22 males and 18 females, with a mean age of 70.3± years. No significant difference in age, sex, weight, height, history of previous surgery, operation time, or anesthesia time were observed between the M group and the CES group.
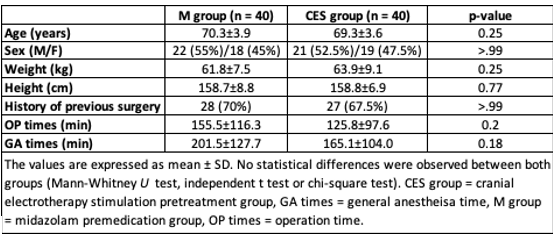
Demographic characteristics of patients in the M and CES groups.
Data Analysis
Anxiety
The anxiety scores in the PHA were significantly lower in the CES group compared with the M group (p = .02). No significant difference was observed in the anxiety scores in the general ward on the night before the surgery and in the OR between the 2 groups.
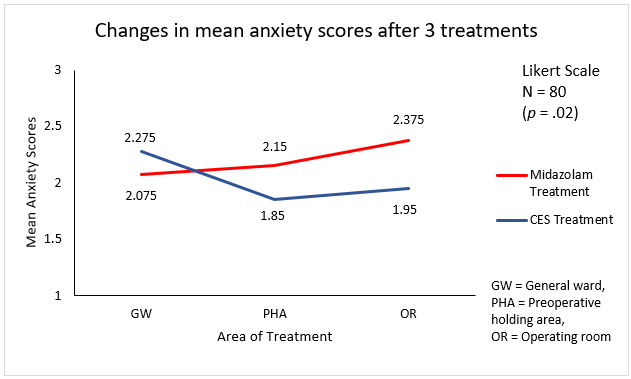
Changes in anxiety scores for the M and CES groups.
Sedation score
The sedation scores in the PHA were significantly lower in the CES group than those in the M group (p < .001). However, no significant difference in the sedation scores was observed in the general ward and OR between the 2 groups.
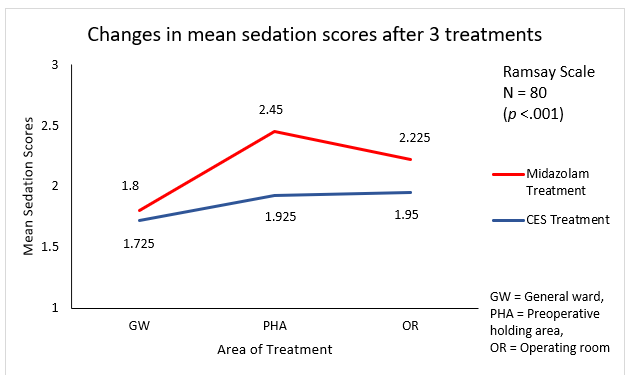
Changes in sedation scores for the M and CES groups.
Vital signs
The M group and the CES group showed no significant differences in systolic, diastolic, and mean blood pressures in the general ward on the night before surgery, in the PHA, and in the OR. No significant difference in HR was observed in the general ward on the night before surgery and in the PHA. However, HRs in the OR were significantly slower in the M group than those in the CES group (M premedication group, 69.2±10.5 beats/min; CES group, 79.6 ±15.3 beats/min) (p < .001).
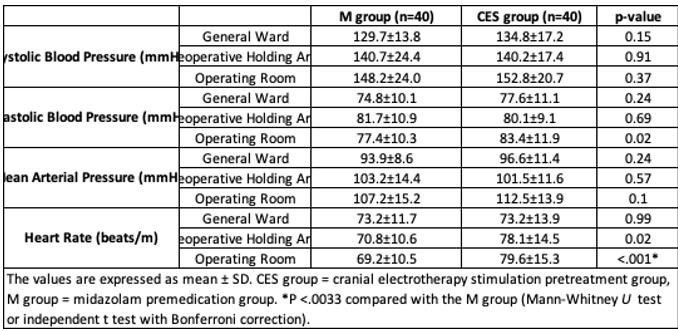
Changes in vital signs for M and CES groups
Finally, the M group and the CES group showed no significant difference in the baseline oxygen saturation in the general ward on the night before. Oxygen saturations in the PHA (M group, 94.3% ± 2.4%; CES group, 97.4% ±1.8%) and the OR (M group, 95.9% ±1.8%; CES group, 97.5% ± 1.6%) were significantly higher in the CES group than those in the M group (p <.001).
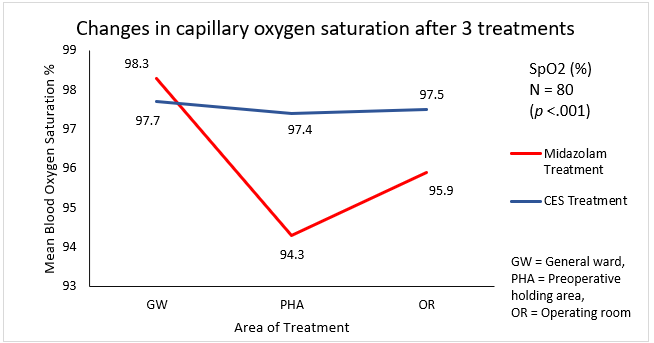
Changes in Oxygen Saturation for M and CES groups
Conclusion
In 65- to 79-year-old patients with American Society of Anesthesiologists Physical Status Classification II or III, CES pretreatment, in comparison with the midazolam premedication, resulted in lower anxiety levels in PHA with less risk of over-sedation and respiratory depression before surgery. Their results showed that pretreatment with CES reduces preoperative anxiety levels and withdrawal responses to rocuronium-induced pain. The study concluded that the noninvasive nature of CES and the absence of serious side effects, indicate it can safely be used on the day before and the day of surgery.
Limitations
The study utilized less than 200 uA of CES for only 20 minutes each. Recommended treatment durations for currents at 200 uA or lower is 60 minutes.
Study Quality: GOOD
