The Constellation Effect – Moving Forward When What May Be Wrong Is a Mystery
By Jeff Jernigan, PhD, BCPPC, FAIS
*This is an article from the Summer 2021 issue of Contentment Magazine.

On April 22, 2021, the keynote speaker at a major global summit unpacked a recent U.S. Department of Commerce projection that globalization will continue to disrupt economies around the world for the next seven years and perhaps longer due to COVID-19.1 “No country will be out of the woods until the world is out of the woods.”2 For employers right down to employees, this means living with uncertainty, varying degrees of health risk, and prolonged stress that will still be with us for some time yet. During this recovery, how do we know if what we are feeling and experiencing is due to the pandemic, or something else? How do we move forward during this confusing time of a literal global transformation?
Unpacking the Mystery
Mary (not her real name) is a 26-year-old working single mother in a residential rehabilitation program for substance use disorder following the death of her husband in an automobile accident in the preceding year. The attending Nurse Practitioner became concerned after a good number of weeks had passed and not all of her physical and psychological symptoms were clearing up. Conditions usually improve when medical and behavioral masking symptoms resolve with growing sobriety. In this case there was continuing depression, panic attacks, excessive fear, angry outbursts, weight loss, recurring intrusive thoughts, incontinence, neuropathy, unresolved rash over most of her body, and migraine headaches. Was it PTSD, an anxiety disorder, depression, profound grief, or the results of a medical condition? I was asked to review the case. My answer was yes, probably part of all of the above.
Sometimes our psychological challenges can become medical conditions through somatization.3 At the same time there may be existing health problems underlying more than one of the symptoms making diagnosis difficult even for healthcare professionals. Many of the conditions Mary was experiencing, including depression, anxiety, anger, mood changes and intrusive thoughts can be symptoms of everything listed in her health record. When there is a veritable constellation of symptoms, especially if some of them are long-term results of a temporary condition, it is very difficult to sort things out. Right now, this is even more difficult due to the stress and isolation associated with COVID-19. Prolonged stress and uncertainty can produce all of these symptoms or none of them.

What makes discerning the cause of our distress is all of the possibilities the pandemic has brought upon us. We live in a very complex time with healthcare risks at an all-time high surrounding us like stars in the sky at night: a constellation of risks to consider. Before we get to some good news answers, let’s get a grasp on just how complex the matter is truly.
Too Many Possibilities
33% of patients hospitalized with COVID-19 receive a neurological or psychiatric diagnosis within six months of recovery. 4 For those patients additionally admitted to an Intensive Care Unit, this jumps to 46%.5 For those of us fortunate enough to have not been infected, the impact of 18 to 24 months of prolonged stress and isolation begins to show up as medical and mental health disorders.6 Loss of concentration, focus, memory, decision making ability and ability to learn from mistakes begins to degrade.7 Headaches, stomach problems, depression and anxiety can increase as well.8 Already we are seeing stress disorders in the U.S. increasing by 26%, anxiety and depression by 31%, Substance Use Disorder up by 13%, and suicides 11% more frequently.9 Mental health difficulties are on the rise in general across the country: 21% of adults experience increased levels of psychological distress.10 34% of these are the result of financial difficulties, and 28% are due to personal health issues.11
For the average person, this news makes it very difficult to know what is behind what we are experiencing. If we are unable to identify a cause, we are also probably unable to do anything about it before we become just another statistic. How do we unravel the complexity and solve the mystery? First, by ruling out what we know are not the problems. In other words, figure out what the cause of our difficulties might be by first eliminating what we know cannot be the cause. Let’s apply this concept to Mary’s situation.
Things to Rule Out
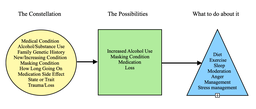
The illustration above includes a number of things to rule out under “Constellation,” some things which, in Mary’s case, cannot be ruled out as “Possibilities,” and some actions Mary may want to consider under “What To Do About It.” Let’s define what we can rule out first. Remember, this is just an example. We are not diagnosing Mary.
- Medical condition: if you have been diagnosed with a medical condition it is best to talk with your doctor concerning other potentially related conditions due to the stress, uncertainty, and isolation of the pandemic.
- Increased or excessive alcohol or controlled substance use: moderation is key. Too much alcohol leads to depression, heightened anxiety, and too much sugar which can trigger excess production of cortisol compromising your immune system.12 The same goes for self-medicating by binge eating or too much junk food. Abusing prescription drugs or other controlled substances is never a good idea. Use medications as prescribed and don’t use prescription medications belonging to someone else.
- Family genetic history: generational trauma can cause changes in the brain including irrational fears, anxiety and worries that can be inherited from your parents or other relatives.13 For example, children and grandchildren of Holocaust survivors have a higher risk of anxiety disorders and PTSD, as do children of 9/11 survivors, as well as children of parents today who are survivors of military combat action in Vietnam, Iraq and Afghanistan. Our own research in Rwanda followed depression, anxiety, and PTSD from the genocide of 1994 into the third generation.14
- New or increasing symptoms: you may have experienced depression or anxiety in the past. However, at present these may be increasing in intensity and frequency. Though you may not know why this is happening, the fact that it is changing is important enough that you cannot rule out anxiety, depression or other past symptoms as commonplace. Any significant change is worth noting.
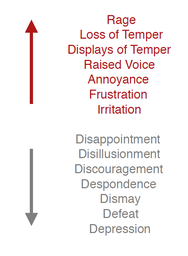
- Masking condition: often one condition can produce another, more visible and predominate condition. One hides the other from view. For example, someone experiencing a significant loss (loss of innocence due to trauma, loss of moral compass, loss of life, loss of relationship, etcetera) can appear to be depressed or anxious, or simply just angry. The anger may be all we see, and it is masking grief and the symptoms associated with grief. Below is an illustration of anger turned inward and turned outward. Notice that it is a spectrum in either direction with different manifestations. We will get back to this point in a moment.
- How long has this been going on? This refers to the length of time you have been experiencing your symptoms. The focus here is the length of time which may be out of proportion to how long you normally experience these symptoms. Stress is cumulative, and if you have not been practicing good stress management it can be suppressed until it shows up physically and psychologically. It never goes away by ignoring it. If you have not been practicing basic stress management, you cannot rule out stress fatigue and related conditions.
- Medications: check the potential side effects of any medications you are taking. If you are taking more than one medication, including over-the counter remedies, check with your doctor or pharmacist for any interactions that might explain your symptoms.
- State or trait: sometimes what we may experience occasionally, even though it repeats itself, may just be a temporary condition. This condition has a measurable beginning and end to it. It is a state that goes away on its own. Headaches are a good example. My allergies give me sinus headaches, but they constitute a state that goes away on its own or with the help of an antihistamine. A trait, on the other hand, is something that comes upon you and doesn’t remit easily. It hangs around for a lot longer, waxing and waning and rarely going away on its own. It is a trait. An example would be people living in parts of the world where the skies are always dreary and gray. Some people thrive in that environment, others struggle with varying degrees of depression until the sun shines again. Yes, it is true, rainy days can really get some of us down as an environmentally induced form of depression.
- Trauma and loss: whether an incident, cluster of incidents, or a constant lower grade of stress over a prolonged period of time, trauma and loss can get us down as well. During the pandemic, it is almost certain we all will experience this to some extent. It can exacerbate other sources of stress and it can mask other underlying health conditions.
Two Things You Can Never Rule Out
In Mary’s case a number of things can be ruled out. Mary was self-medicating with alcohol. The amount was not significant, but the conditions of her residential treatment program prohibited the consumption of any alcohol, and she felt embarrassed and ashamed. This only added to her difficulties responding to the tragic loss of her husband and her inability to struggle well with the grief naturally involved.
Anger is a large part of grief and provided the first clue that it may be masking something else. Because grief is normally expected following trauma and loss, no one looked further. However, grief prolonged can make the heart sick. Mary was experiencing what is called Profound Grief or Complicated Grief Disorder.15 Mary was also taking antidepressant and anti-anxiety medication. Sometimes this pairing, depending on the specific medications, can create a dangerous cycle. She took an antidepressant in the morning. By late afternoon she began to experience some anxiety, a side effect of some antidepressants. So, she took her anti-anxiety medication which, you guessed it, produced a slight sense of depression by morning. Her medication needed to be adjusted to eliminate this addictive cycle and eliminate the side effects.
Once her medication was adjusted, she began to get help for managing her grief, and committed herself to abstaining from alcohol. Things improved tremendously. But even with attention given to nutrition, exercise, and sleep along with some stress management skill development, she was still an angry person. This is because anger, in its various forms, is a part of our daily lives even if we are not aware of it.
Most of us do not have the life complications Mary is struggling with in this illustration. Her experience is a good example of how complicated and confusing things can become. Most of what she is experiencing is highly situational. However, there are two things she is experiencing that we all experience as well, things which do not ever go away and therefore cannot be ruled out. However, they certainly can be managed well: anger and stress.
Anger is a healthy emotion, but if not tamed can be very destructive physiologically and psychologically for you and for others around you. Anger is both a feeling and a choice; emotion and volition. Even though the choice may have been automatic and unnoticed, neurologically it happened. That means we can choose not to be angry as well. Anger turned inward is usually the result of feeling impotent, powerless, even hopeless with no one to blame, no one to hold responsible, and no one to remove the sense of fear and vulnerability it creates. The result can be a spectrum of emotions from disappointment to depression. Anger expressed outwardly can range from irritation to rage in response to alienation of real or perceived rights, injustice suffered, or outrage over betrayed values. In either case, the foundation of anger is found in disappointed expectations, frustrated desires, and blocked goals.
Finding Helpful Answers
Solving the mystery of our experience during trying times (and these are trying times) is a process not an event. Begin with a strategic perspective: how am I doing managing stress in my life? Am I balancing stretching experiences with nourishing ones; in control of my diet, exercise, and sleep; investing in a few close relationships; taking regular breaks instead of plowing through things? Am I an angry person? Are there disappointed expectations, frustrated desires, or blocked goals I am holding onto? Do I find myself sensitive, easily provoked, irritated more than usual? Am I able to identify these things to the point I can respond constructively, or therapeutically release them? Now we can get tactical, looking for more specific things to rule out.
Do what you can to resolve or manage what is left. Just being able to label these things will bring its own relief. Our tomorrows will be what we make them.
“Yesterday, when it was tomorrow, it was too much day for me,” Winnie the Pooh.16
References
- Vyas, N., The Impact of COVID-19 on Global Supply Chain Management and Logistics: University of Southern California, Marshall School of Business; Keynote address at the 62nd Annual Global Summit, Stanton Chase International, April 2021
- Ibid
- American Psychiatric Association, Somatic Symptoms and Related Disorders: Diagnostic and Statistical Manual of Mental Disorders DSM-5, American Psychiatric Association, 2013, PP 309-327
- Taquet, M., Geddes, R., Husain, M., Luciano, S., Harrison, P.; Neurological and Psychiatric Morbidity Following Covid-19: The Lancet Psychiatry, DOI:https://doi.org/10.1016/S2215-0366(21)00084-5, April 2021
- Ibid
- Jernigan, J.; Recovery Through Workplace Engagement: Stanton Chase Global White Paper, https://www.stantonchase.com/recovery-through-workplace-engagement/, March 2021
- Ibid
- Ibid
- Czeisler, M. E., Lane, R.I., Petroskey, E.; Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic – United States: MMWR Morb MortalWeekly Report, 2020:69-1049-1057
- Keeter, S; Many Americans Continue to Experience Mental Difficulties as Pandemic Enters Second Year: Fact-Tank, Pew Research Center, March 2021
- Ibid
- Thau, L., Gandi, J., Sandeep, S.; Replication of Cortisol Circadian Rhythm: New Advances in Hydrocortisone Replacement Therapy: Physiology, Cortisol; StatPearls Publishing 2021
- Amen, D.; Meet the Ancestral Dragons that Haunt Generations: amenclincs.com, March 2021
- Jernigan, J., Jernigan, N.; Mental Health in Rwanda: Pioneer Research Report; HVG, Olive Branch International, Rwanda Ministry of Health
- Mayo Clinic Staff, Symptoms and Causes: Complicated Grief: Mayo Clinic https://www.mayoclinic.org/diseases-conditions/complicated-grief/symptoms-causes/syc-20360374?p=1, 2021
- Milne, A. A., Shepherd, E. H.; Winnie-The-Pooh: Dutton, 2001
ABOUT THE AUTHOR

Jeff Jernigan, PhD, BCPPC, FAIS is a board-certified mental health professional known for influencing change in people and organizations by capitalizing on growth and change through leadership selection and development. Jeff currently serves Stanton Chase Pacific as the regional Life-Science and Healthcare Practice Leader for retained executive search and is the national subject matter expert for psychometric and psychological client support services.
A lifetime focus on humanitarian service is reflected in Jeff’s role as the Chief Executive Officer and co-founder, with his wife Nancy, for the Hidden Value Group, an organization bringing healing, health, and hope to the world in the wake of mass disaster and violence through healthcare, education, and leadership development. They have completed more than 300 projects in 25 countries over the last 27 years. Jeff currently serves as a Subject Matter Expert, Master Teacher, Research Mentor, or Fellow in the following professional organizations: American Association of Suicidology, National Association for Addiction Professionals, The American Institute of Stress, International Association for Continuing Education and Training, American College of Healthcare Executives and the Wellness Council of America.
Contentment Magazine
The dictionary defines “content” as being in a state of peaceful happiness. The AIS magazine is called Contentment because we want all of our guests and members to find contentment in their lives by learning about stress management and finding what works best for each them. Stress is unavoidable, and comes in many shapes and sizes that makes being in a state of peaceful happiness seem like a very lofty goal. But happiness is easy to find once you are able to find ways to manage your stress and keep a healthy perspective when going though difficult times in life. You will always have stress, but stress does not always have you!
