*This is an article from the Winter 2022 issue of Contentment Magazine.
By Rita Hitching BSc, MSc, PhD Candidate
Christopher Gordon BN, PhD
Lisa Lampe MBBS, PhD, FRANZCP
In 1789, one of our most influential Founding Fathers — Benjamin Franklin (1706-1790) — famously wrote, “…In this world, nothing is certain except death and taxes.” I would argue that if Franklin were alive today, he would probably have said “… In this world, nothing is certain except death, taxes, and stress…”
In this article, we demonstrate the relationship between stress and sleep disturbance and explore how technology, previously criticized as being the trigger for our high-stress living, is being used for good. We also highlight how the emerging application of Virtual Reality is helping ensure you get a good night’s sleep by facilitating the delivery of existing treatments such as mindfulness.
How Does Stress Impact Health?
Statistics from the CDC show that even before the stress associated with the pandemic, more than 60 million Americans reported chronic sleep difficulties.1 Since then, rising inflation and living costs, and global uncertainty, including the invasion of Ukraine, have escalated stress levels even further. A 2021 Stress in America survey by the American Psychological Association reports that regardless of age, background, or walk of life every American is suffering.2 Persistent stressors such as difficulties at work, family or relationship problems, and financial worries are known risk factors for disease and premature death.3 One of the lesser-known ways chronic stress impacts physical and mental health is through the disruption of our body’s principal restorative tool – sleep.
What can be described as stress varies enormously, but from a physiological perspective the cocktail of chemicals your body mixes in response to it is the same. Any stimulus or stressor — physical or psychological — if potentially harmful or even just challenging will elicit a stress response. The stress system begins with the activation of two discrete physiological mechanisms: the sympathetic-adreno-medullary (SAM) axis releasing adrenaline (epinephrine) and noradrenaline (norepinephrine) and the hypothalamic–pituitary–adrenal (HPA) axis releasing glucocorticoids such as cortisol. The elevated cortisol levels that are part of the fight or flight stress response promote alertness and inhibit sleep. What this coordinated response accomplishes is a readiness for fight or flight by promoting metabolic changes and mobilizing energy sources with notable increases in heart and breathing rates and glucose release.
To maximize a prompt and concerted response to overcome the perceived challenge the body also suppresses the digestive, reproductive, and immune systems. If you have ever wondered why being stressed makes you more likely to catch a cold, get an upset tummy, or make you lose interest in your nearest and dearest — now you know why! The body’s brilliant lifesaving stress response places a lot of physiological demands, often before, during, and after a stressful situation. If you just responded to an emergency or finished a big presentation — once the immediate ‘danger’ is out of the way — you feel ready to collapse into a heap. You might even feel like you need to lie down or take a nap!
Is Stress the Cause of Disrupted Sleep?
Exactly how stress impairs our ability to sleep remains unclear, but stressful life events have long been known to trigger sleep disorders, most commonly insomnia. One thing we do know is that our body’s response to stress shares the same brain pathways with those that govern our sleep-wake cycle – the HPA axis.
The acute or short-term stressors associated with day-to-day life may prevent you from getting a good night’s sleep every now and then, but do not typically result in persistent sleep difficulties. In contrast, the persistently high cortisol levels attributed to the relentless activation of the stress response by ongoing or chronic stressors contribute to the dysregulation of the HPA axis by reducing its sensitivity to cortisol and inhibiting the release of melatonin associated with sleep onset. Chronic stress also appears to change the very architecture of sleep. When you are stressed, you spend less time in the restorative zone of sleep known as slow wave and rapid eye movement (REM) sleep. The impact of stress on sleep goes even further, influencing the emotional content and patterns of dreaming.
Why Does Sleep Matter?
Like stress, insomnia is highly prevalent and associated with significant economic and healthcare burden, morbidity, and mortality. Insufficient sleep costs the US economy $411 billion each year in lost productivity (reduced employment, premature death, absenteeism, and presenteeism).4 The pervasive nature of sleep disorders, in particular, insomnia has been referred to as a ‘global epidemic’ by the World Health Organization.5

 Sleep is critical to health and wellbeing because it enables our bodies and importantly, our brains to rest, repair, and rejuvenate. The strength of the relationship between chronic stress and sleep disturbance is underscored by the strong associations they share with common health conditions such as type II diabetes and obesity, cardiovascular disease and hypertension, Parkinson’s and Alzheimer’s diseases, stroke, and chronic pain. Disrupted sleep impairs memory and attention, learning and problem-solving abilities, and increases the risk of accidents and injuries, particularly motor vehicle accidents. Quality of life is reduced when sleep difficulties persist. In addition, insomnia or poor sleep is known to increase the risk of psychiatric disorders such as depression and anxiety and may contribute to relapse and impede recovery. Insomnia is a strong risk factor for suicide and a more powerful predictor than depression.6,7
Sleep is critical to health and wellbeing because it enables our bodies and importantly, our brains to rest, repair, and rejuvenate. The strength of the relationship between chronic stress and sleep disturbance is underscored by the strong associations they share with common health conditions such as type II diabetes and obesity, cardiovascular disease and hypertension, Parkinson’s and Alzheimer’s diseases, stroke, and chronic pain. Disrupted sleep impairs memory and attention, learning and problem-solving abilities, and increases the risk of accidents and injuries, particularly motor vehicle accidents. Quality of life is reduced when sleep difficulties persist. In addition, insomnia or poor sleep is known to increase the risk of psychiatric disorders such as depression and anxiety and may contribute to relapse and impede recovery. Insomnia is a strong risk factor for suicide and a more powerful predictor than depression.6,7
What Treatments Are Available?
Growing public concern about the health impact of poor sleep has resulted in increased demand for effective strategies to help us get a good night’s sleep. Considering the relationship between stress and disrupted sleep, approaches that minimize the impact of chronic stress like regular exercise (preferably outdoors), low fat/sugar diets, and the avoidance of caffeine, nicotine, and alcohol are central to addressing sleep difficulties.
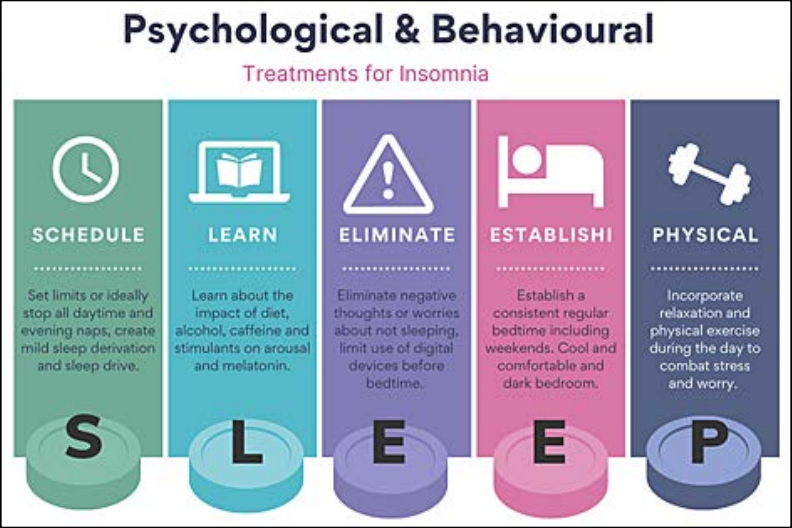
First-line approaches include behavioural modifications such as sleep hygiene and limiting daytime naps to support the sleep-wake cycle in concert with cognitive therapies that target the thoughts that often contribute to sleep problems. (See Figure 1). In addition to adopting strategies that counteract the effects of stress in our life, including our sleep, finding ways to gain greater control over our actions and their consequences means even highly stressful situations like a chronic illness or relationship problems become more manageable.
Insert Figure 1: HitchingGordonLampe_Infographic.tiff (Caption below)
Figure 1: Behavioural & Cognitive Modifications to Support Insomnia
Can Technologies Like VR Be Used to Facilitate Sleep?
As our understanding that even small lifestyle changes can have powerful short and long-term impacts on our health has grown, so has the demand for tools8 to help us track our daily activities and facilitate behavioural change.9,10 Available tools have been greatly aided by advances in modern technology that facilitate human-computer interactions (HCI), the same modern technology that at times has been considered a catalyst for stress and a contributor to poor sleep – the smartphone and social media.
HCI tools to help you take control of your wellbeing are being incorporated into a burgeoning array of hardware and software options11 including smartwatches that track your sleep, bed pads and pillows that keep you cool, glasses to block blue light, yellow light bulbs to stimulate melatonin secretion, sunrise alarm clocks, weighted blankets, noise-cancelling earbuds that also transmit nature sounds, wrist bands that measure stress levels and remind you to “calm down and relax”, headbands to support deep sleep, and meditation and mindfulness apps to help manage stress, reduce anxiety, and promote sleep.
Some of these tools and devices are adding other HCI interfaces like Virtual Reality (VR), typically associated with the entertainment and gaming industry to enhance their therapeutic offering12. The new generation of VR is accessible via inexpensive, lightweight, easy to use, and highly portable smartphones, that use low-cost optics, and pre-warp images to deliver high-quality crisp graphics that are remarkably immersive and can be viewed using VR helmets without the need for hardwiring to fast and expensive gaming computers. The immersive three-dimensional world of VR creates a feeling of being in a new world or reality, rather than viewing it on a screen. Users can interact with the virtual world enabling experiences like to feel more realistic.
The neurobehavioral mechanisms of action of digital technologies like VR are still unclear, but VR is associated with changes to cortical activity principally in the anterior cingulate cortex and the orbitofrontal region of the brain. How the process occurs is largely unknown, but thought to be attributed to stimulation of the visual cortex through the pathways of the optic nerve during immersion.12
VR13 has been used to augment the delivery of existing treatments such as exposure therapy (ET) and cognitive behavioural therapy (CBT) for disorders that frequently show vulnerability to chronic stress such as PTSD, social anxiety, OCD, depression, and ADHD.14 VR is also being used to offer real-time biofeedback in conjunction with other behavioural approaches to target psychiatric disorders that frequently include insomnia as a presenting symptom.15 The overlapping nature of chronic stress, psychiatric symptoms, and sleep should not come as a surprise when you consider that the neural pathways that regulate stress also regulate sleep, and regulate mood and anxiety.16
The success of VR at targeting disorders commonly associated with poor sleep is paving the way for research exploring its potential for the treatment of insomnia. Critical to being able to fall asleep is the ability to feel relaxed and calm. VR has already been shown to reduce physiological, psychological, and biochemical stress indicators known to contribute to insomnia.17 Consequently, a promising application of VR is targeting hyperarousal18 (elevated heart rate and blood pressure, cortical activity,19, 20 and anxiety) common in insomnia. 21, 22
Leveraging VR’s capacity to capture focused attention by excluding and immersing the user in a calm and peaceful virtual world, may augment the proven benefits of traditional relaxation techniques that are central to evidence-based treatments for insomnia like CBT.22 VR therapies are expected to result in greater modulation of arousal levels to facilitate sleep onset more effectively than traditional relaxation techniques.23
The use of VR relaxation before sleep has led to sustained reductions in hyperarousal and self-reported levels of worry24 – known to contribute to insomnia.25 In addition to amplifying the benefits of relaxation, VR has been shown to improve sleep quality26 by reducing the number of awakenings and sleep stage transition.22, 26 In addition, the use of a virtual lullaby machine that combines a mix of ambient music with dynamic kaleidoscopic visuals has been shown to reduce cognitive arousal or drown out thoughts and induce sleepiness.27 If this idea of a virtual lullaby sounds appealing, similar commercially available options can be found in the App store.

Although the application of VR for sleep is still in its early stages and more research is needed, the preliminary findings are showing promise. VR offers the potential for engaging personalized environments that can provide real and lasting therapeutic benefits. It just might be time to buy a VR headset.
References
- Wheaton A, Everett Jones S, Cooper A, Croft J. Short Sleep Duration Among Middle School and High School Students — United States, 2015 [Internet]. Centers for Disease Control and Prevention; 2018 [cited 2022 Aug 16] p. 85–90. (MMWR Morb Mortal Wkly Rep 2018). Report No.: 67. Available from: https://www.cdc.gov/mmwr/volumes/67/wr/mm6703a1.htm
- American Psychological Association. Stress in America 2021: Stress and Decision-Making During the Pandemic. 2021.
- Mariotti A. The effects of chronic stress on health: new insights into the molecular mechanisms of brain–body communication. Future Sci OA. 2015 Nov 1;1(3):FSO23.
- Hafner M, Stepanek M, Taylor J, Troxel WM, van Stolk C. Why Sleep Matters-The Economic Costs of Insufficient Sleep: A Cross-Country Comparative Analysis. Rand Health Q. 2017 Jan;6(4):11.
- Chattu VK, Manzar MD, Kumary S, Burman D, Spence DW, Pandi-Perumal SR. The Global Problem of Insufficient Sleep and Its Serious Public Health Implications. Healthcare. 2019 Mar;7(1):1.
- Faccini J, Joshi V, Graziani P, Del-Monte J. Non-Constructive Ruminations, Insomnia and Nightmares: Trio of Vulnerabilities to Suicide Risk. Nat Sci Sleep. 2022 Mar 15;14:433–41.
- Bernert RA, Kim JS, Iwata NG, Perlis ML. Sleep disturbances as an evidence-based suicide risk factor. Curr Psychiatry Rep. 2015 Mar;17(3):554.
- Lecomte T, Potvin S, Corbière M, Guay S, Samson C, Cloutier B, et al. Mobile Apps for Mental Health Issues: Meta-Review of Meta-Analyses. JMIR MHealth UHealth. 2020 May 29;8(5):e17458.
- Marshall PWM, Schabrun S, Knox MF. Physical activity and the mediating effect of fear, depression, anxiety, and catastrophizing on pain related disability in people with chronic low back pain. PLoS ONE. 2017 Jul 7;12(7):e0180788.
- Western MJ, Armstrong MEG, Islam I, Morgan K, Jones UF, Kelson MJ. The effectiveness of digital interventions for increasing physical activity in individuals of low socioeconomic status: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2021 Nov 9;18(1):148.
- Torous J, Bucci S, Bell IH, Kessing LV, Faurholt-Jepsen M, Whelan P, et al. The growing field of digital psychiatry: current evidence and the future of apps, social media, chatbots, and virtual reality. World Psychiatry. 2021;20(3):318–35.
- Colloca L, Raghuraman N, Wang Y, Akintola T, Brawn-Cinani B, Colloca G, et al. Virtual reality: physiological and behavioral mechanisms to increase individual pain tolerance limits. Pain. 2020 Sep 1;161(9):2010–21.
- Dellazizzo L, Potvin S, Luigi M, Dumais A. Evidence on Virtual Reality–Based Therapies for Psychiatric Disorders: Meta-Review of Meta-Analyses. J Med Internet Res. 2020 Aug 19;22(8):e20889.
- Maples-Keller JL, Bunnell BE, Kim SJ, Rothbaum BO. The Use of Virtual Reality Technology in the Treatment of Anxiety and Other Psychiatric Disorders. Harv Rev Psychiatry. 2017 Jun;25(3):103–13.
- Kothgassner OD, Goreis A, Bauda I, Ziegenaus A, Glenk LM, Felnhofer A. Virtual reality biofeedback interventions for treating anxiety. Wien Klin Wochenschr. 2022 Jan 1;134(1):49–59.
- Palagini L, Miniati M, Riemann D, Zerbinati L. Insomnia, Fatigue, and Depression: Theoretical and Clinical Implications of a Self-reinforcing Feedback Loop in Cancer. Clin Pract Epidemiol Ment Health [Internet]. 2021 Dec 31 [cited 2022 Mar 31];17(1). Available from: https://clinical-practice-and-epidemiology-in-mental-health.com/VOLUME/17/PAGE/257/ABSTRACT/
- Mazgelytė E, Rekienė V, Dereškevičiūtė E, Petrėnas T, Songailienė J, Utkus A, et al. Effects of Virtual Reality-Based Relaxation Techniques on Psychological, Physiological, and Biochemical Stress Indicators. Healthc Basel Switz. 2021 Dec 14;9(12):1729.
- Lechat B, Appleton S, Melaku YA, Hansen K, McEvoy RD, Adams R, et al. The association of co-morbid insomnia and sleep apnea with prevalent cardiovascular disease and incident cardiovascular events. J Sleep Res. 2022 Feb 15;e13563.
- Miller CB, Bartlett DJ, Mullins AE, Dodds KL, Gordon CJ, Kyle SD, et al. Clusters of Insomnia Disorder: An Exploratory Cluster Analysis of Objective Sleep Parameters Reveals Differences in Neurocognitive Functioning, Quantitative EEG, and Heart Rate Variability. Sleep. 2016 Nov 1;39(11):1993–2004.
- Levenson JC, Kay DB, Buysse DJ. The Pathophysiology of Insomnia. Chest. 2015 Apr;147(4):1179–92.
- Bonnet MH, Arand DL. Hyperarousal and insomnia: state of the science. Sleep Med Rev. 2010 Feb;14(1):9–15.
- Zambotti M de, Sizintsev M, Claudatos S, Barresi G, Colrain IM, Baker FC. Reducing bedtime physiological arousal levels using immersive audio-visual respiratory bio-feedback: a pilot study in women with insomnia symptoms. J Behav Med. 2019 Oct 1;42(5):973–84.
- Zambotti M, Barresi G, Colrain IM, Baker FC. When sleep goes virtual: the potential of using virtual reality at bedtime to facilitate sleep. Sleep [Internet]. 2020 Dec 1 [cited 2021 Sep 20];43(12). Available from: https://doi.org/10.1093/sleep/zsaa178
- Yüksel D, Goldstone A, Prouty D, Forouzanfar M, Claudatos S, Lee Q, et al. The Use of Immersive Virtual Reality and Slow Breathing to Enhance Relaxation and Sleep in Adolescents. Sleep. 2020 Apr;43:A348.
- Weiner L, Martz E, Kilic-Huck Ü, Siegel N, Bertschy G, Geoffroy PA, et al. Investigating racing thoughts in insomnia: A neglected piece of the mood-sleep puzzle? Compr Psychiatry. 2021 Nov 1;111:152271.
- Lee SY, Kang J. Effect of virtual reality meditation on sleep quality of intensive care unit patients: A randomised controlled trial. Intensive Crit Care Nurs. 2020 Aug 1;59:102849.
- Semertidis, NA, et al., Towards Understanding the Design of Positive Pre-Sleep Through a Neurofeedback Artistic Experience. CHI. 2019, May: 4–9 Available at: https://exertiongameslab.org/wp-content/uploads/2019/04/towards_pre_sleep_chi2019.pdf.
ABOUT THE AUTHOR

Associate Lecturer at the University of Newcastle School of Medicine and Public Health, Rita Hitching is completing her PhD exploring how virtual reality may be used to deliver insomnia treatment to modulate the bidirectional relationship between disordered sleep, brain function, and psychiatric disorders. She is a well-respected writer and the editor of Briefing Books at the Association for Behavioural & Cognitive Therapies.
University of Newcastle School of Medicine and Public Health Associate Professor and Deputy Head of School, Lisa Lampe, is an academic psychiatrist with a research and clinical focus on anxiety disorders and related symptoms, and treatment using cognitive behavioural therapy. She is a respected educator in the undergraduate, postgraduate, and continuing medical education spaces. She has written books, educational modules, and workshops for academic, healthcare professionals and general audiences. Lisa maintains an active involvement in consumer and career support organisations.
research and clinical focus on anxiety disorders and related symptoms, and treatment using cognitive behavioural therapy. She is a respected educator in the undergraduate, postgraduate, and continuing medical education spaces. She has written books, educational modules, and workshops for academic, healthcare professionals and general audiences. Lisa maintains an active involvement in consumer and career support organisations.
Associate Professor Christopher Gordon is a Research Leader of Insomnia and Chronobiology at the Woolcock Institute of Medical Research and the Faculty of Medicine and Health, University of Sydney. He leads a multidisciplinary insomnia research program focusing on understanding the pathophysiology of insomnia and conducting randomised controlled trials of digital insomnia therapies and non-pharmacological chronotherapies for the treatment of circadian rhythm disruptions.
of Medicine and Health, University of Sydney. He leads a multidisciplinary insomnia research program focusing on understanding the pathophysiology of insomnia and conducting randomised controlled trials of digital insomnia therapies and non-pharmacological chronotherapies for the treatment of circadian rhythm disruptions.
Contentment Magazine
The dictionary defines “content” as being in a state of peaceful happiness. The AIS magazine is called Contentment because we want all of our guests and members to find contentment in their lives by learning about stress management and finding what works best for each them. Stress is unavoidable, and comes in many shapes and sizes that makes being in a state of peaceful happiness seem like a very lofty goal. But happiness is easy to find once you are able to find ways to manage your stress and keep a healthy perspective when going though difficult times in life. You will always have stress, but stress does not always have you!

Leave A Comment
You must be logged in to post a comment.